Artificial General Intelligence for Radiation Oncology
Multimodal Data in Radiation Oncology: A Game-Changer for Patient Care
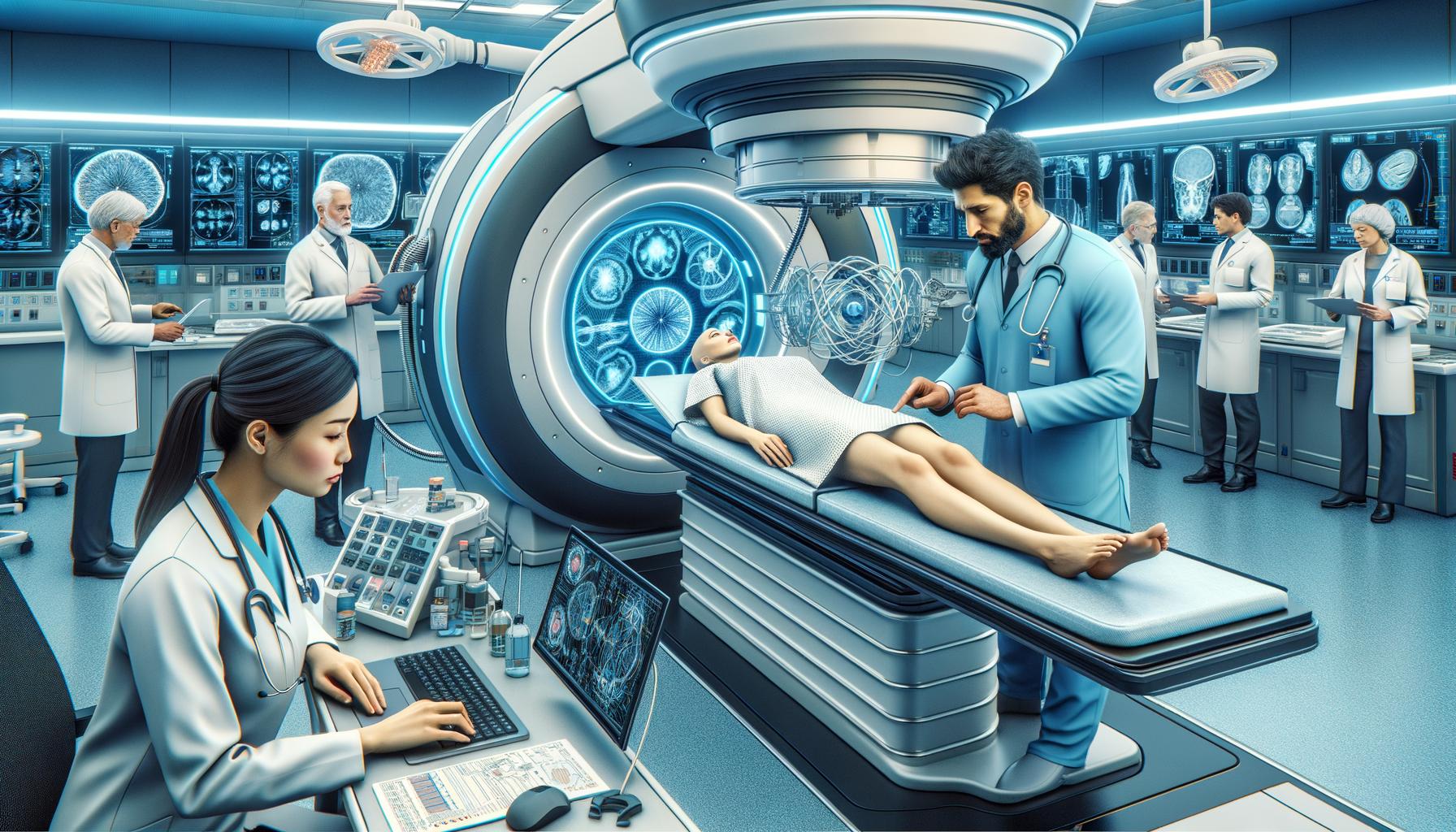
Radiation oncology plays a crucial role in the treatment of cancer patients, with radiotherapy being an effective option for nearly 50-70 percent of them. Traditional radiotherapy involves multiple stages, from consultation to treatment delivery. However, with the rise of Artificial Intelligence (AI), radiotherapy is undergoing a significant transformation. AI, particularly Artificial General Intelligence (AGI), has the potential to elevate the standard of patient care in radiation oncology by exploiting multimodal clinical data at scale.
The Impact of Artificial General Intelligence on Radiation Oncology
AGI is poised to revolutionize radiation oncology by offering advanced capabilities in few-shot and zero-shot learning. Pioneering AGI models, like GPT-4 and PaLM 2, have demonstrated their ability to process extensive texts and imaging data, respectively. These models achieve human-level accuracy in auto-segmentation, tumor staging, image registration, automatic treatment planning, quality assurance, and outcomes prediction. AGI’s integration into radiation oncology can improve the accuracy, precision, and efficiency of radiation therapy, ultimately enhancing patient outcomes.
AGI Models for Improved Precision and Efficiency in Radiotherapy
AGI models have the potential to transform the field of radiation oncology by providing highly robust and generalizable AI models. These models can complement human expertise and care, leading to data-driven, personalized radiation therapy. For example, AGI models can assist in accurate tumor delineation, which is crucial for precise treatment planning. By leveraging multimodal data, AGI enables comprehensive analysis, allowing clinicians to make informed decisions and tailor treatment strategies for individual patients. This personalized approach can significantly enhance the effectiveness of radiation therapy.
Integrating Vision Data with LLMs: Creating Powerful Multimodal Models
Researchers have found that the fusion of vision data with Large Vision Models (LLMs) creates powerful multimodal models that uncover intricate clinical patterns. Advanced AGI models, such as SAM (Segment Anything Model), can process imaging data efficiently, enabling better identification and analysis of tumor characteristics. By combining imaging data with textual information, these multimodal models provide a comprehensive understanding of the patient’s condition, facilitating targeted treatment planning. The integration of vision data with AGI models paves the way for seamless and effective integration into all aspects of radiation oncology.
Future Directions of AGI in Radiation Oncology: Advancements and Challenges Ahead
The future of AGI in radiation oncology holds tremendous potential for advancements in clinical applications. These advancements will further enhance the effectiveness of radiation therapy, resulting in more positive outcomes for cancer patients. However, there are challenges that need to be addressed. The development of AGI models requires extensive data collection and annotation, which can be time-consuming and resource-intensive. Additionally, ensuring the ethical and responsible use of AGI in patient care is crucial. As the field progresses, there is a need for collaboration between clinicians, researchers, and AI experts to overcome these challenges and harness the full potential of AGI in radiation oncology.
In conclusion, AGI has the power to transform radiation oncology by leveraging multimodal clinical data and creating highly robust and generalizable AI models. The integration of AGI into radiation therapy can improve precision, efficiency, and personalized treatment planning, elevating the standard of patient care. While advancements are being made, addressing challenges such as data collection, ethics, and responsible use is crucial for the successful implementation of AGI in radiation oncology. With further research and collaboration, AGI holds the key to revolutionize cancer treatment and bring hope to patients worldwide.
Analyst comment
This news can be evaluated as positive. As an analyst, it is predicted that the integration of Artificial General Intelligence (AGI) into radiation oncology will lead to improved precision, efficiency, and personalized treatment planning in radiotherapy. The use of AGI models can enhance the accuracy of tumor delineation, enable comprehensive analysis of patient data, and facilitate targeted treatment strategies. However, challenges such as data collection, ethics, and responsible use need to be addressed for successful implementation. Collaborative efforts among clinicians, researchers, and AI experts are crucial for harnessing the full potential of AGI in radiation oncology.